“It’s just common sense,” says Dr. Paul Marik.
Stop the presses.
We now have peer-reviewed, scientific proof that bears irrefutable, evidentiary witness to what the physicians of the FLCCC and others have known — and shared widely — since the start of the pandemic: Early combination treatment for COVID-19 decreases fatality rates.
Who knew?
We did. Others did. Honduras sure did. And YOU did too if you were listening. (Or if the presses had really been rolling on this.)
It’s just basic medical common sense. Let’s call it, ‘Treating COVID Early 101.’ Kind of like when you get a cold, you may take a decongestant or an aspirin to lessen the chance that it will escalate into something more serious. Or when you have an upset stomach, you may take an anti-diarrheal to get things under control before dehydration or other, more dire, conditions develop. Like that.
So get this: Soon after the start of the pandemic, Honduran physicians implemented what some consider to be a ‘novel approach’ to tackling COVID. It was based on the following hypothesis: By using an early protocol of highly safe, FDA-approved, repurposed, inexpensive medications known to aid in the reduction of lung inflammation, immune system disruption and clotting in both in-patients and out-patients, deaths from COVID would decrease.
Guess what? They did.
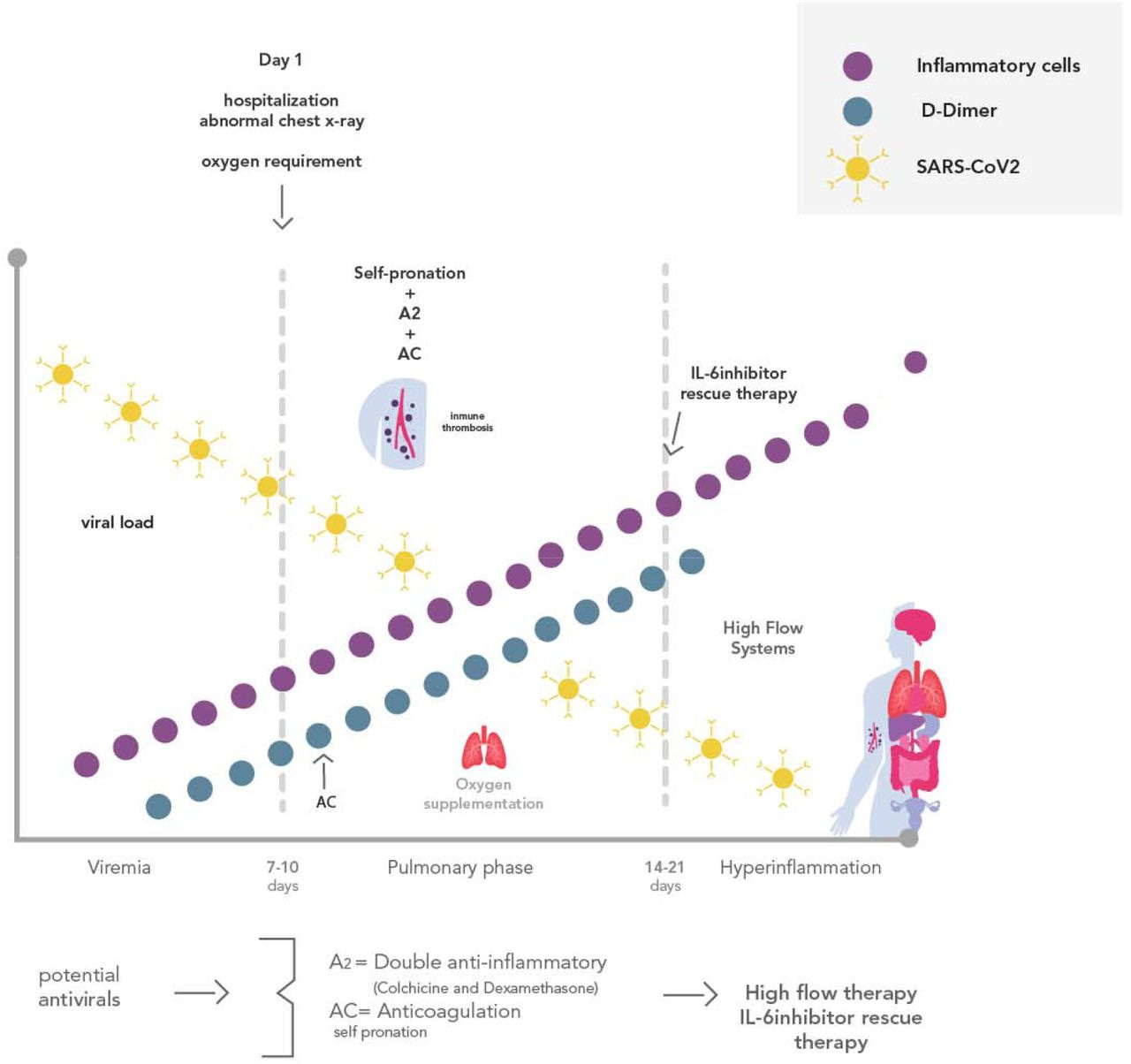
In a new study conducted by a team of physicians and epidemiologists in Honduras, the results showed that fatality rates decreased significantly among both in-patients and out-patients who received early combination treatment for COVID-19. Within two months of the start of the pandemic in the spring of 2020, the Honduran government began to champion nationwide early combination therapy. The components of the protocols included several interventions known for their anti-viral, anti-inflammatory or anticoagulation properties. These drugs included corticosteroids, colchicine, ivermectin, zinc, azithromycin, and low molecular weight heparin.
“My one mantra over the past two years has been that this is a highly treatable disease,” said Dr. Pierre Kory. “The greatest successes around the world are those places, like Honduras, that used early treatment protocols.”
Honduras took this bold action to save its citizens based on the recommendations of an advisory team of critical care and infectious disease specialists. The country had only 19 critical care physicians and 125 ICU beds to support 9.9 million people — and at the time it was still reeling from an epidemic of dengue fever. That’s why doctors in Honduras believed their national healthcare system was in imminent danger of collapse; fearful that COVID would swiftly overwhelm all existing medical resources.
Working with the government, the advisory team of physicians believed if they could stop the progression of the cytokine storm, immune suppression and the clotting that escalates even after the cessation of viral replication with combination therapy (also known as MMA—Multi-Mechanism Approach), they could dramatically decrease fatalities and ICU admissions.
However, they did not have time to wait to prove their theory before acting. They had to move quickly — trusting what their collective clinical expertise and medical knowledge was telling them: This therapy will work. The virus wasn’t going to patiently wait around while a long-term, randomized controlled double-blind study was conducted to test the efficacy of what the doctors had proposed.
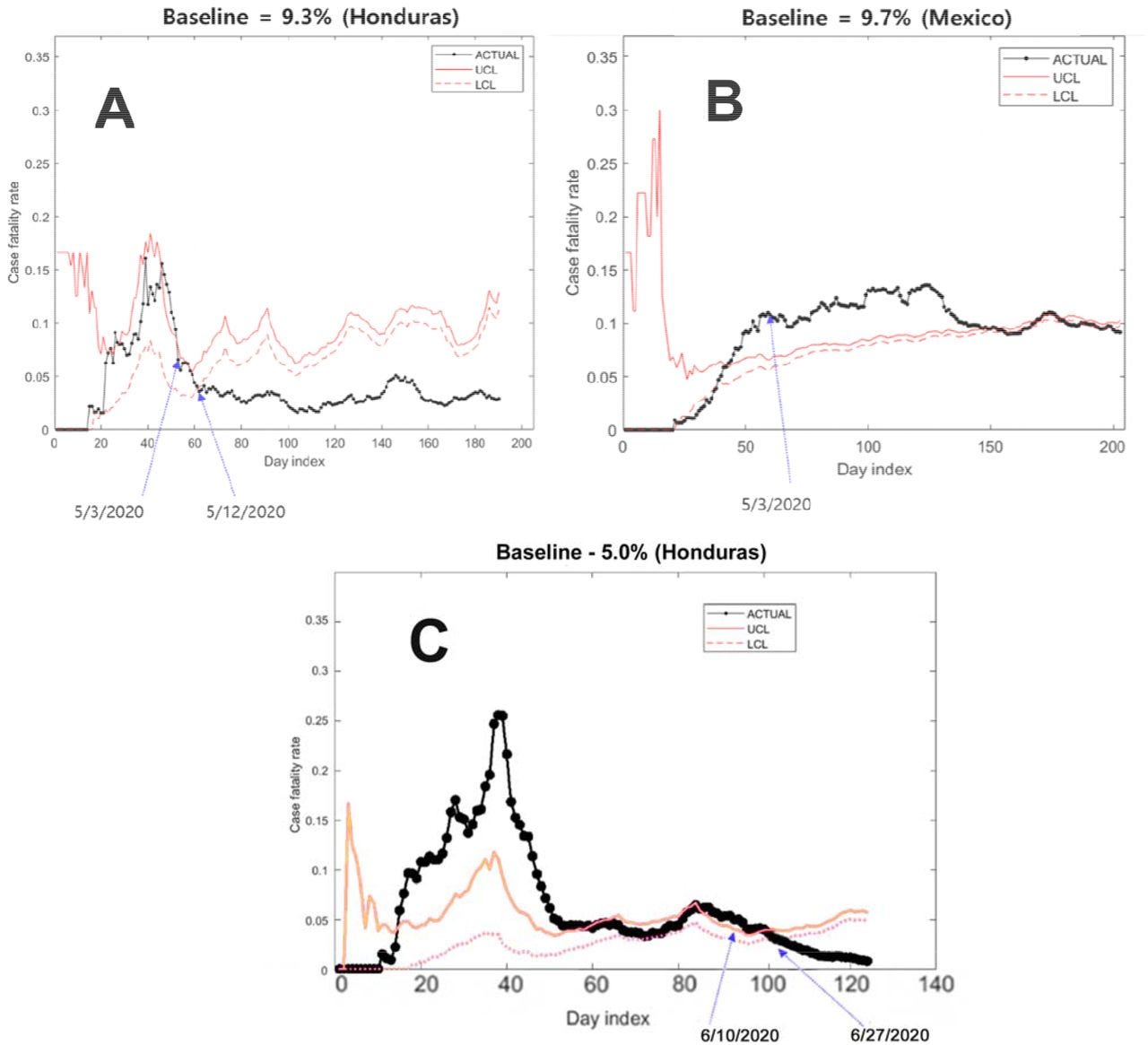
So instead, they decided to implement a methodology known as Statistical Process Control (SPC). Developed over a century ago to improve productivity in manufacturing, SPC has gained wider acceptance in the field of healthcare over the decades. SPC achieves statistical significance through frequent measurements over time.
Using SPC, the research team created control charts to compare COVID-19 case fatality rates in Honduras with those in a control country, Mexico. Mexico was the ideal control country since it had a population of comparable age, demographics, and socio-economic status. Mexico’s climate was also similar to that of Honduras, as were their case fatality rates.
On May 3, 2020, the Honduran Department of Health gave the green light to physicians to begin implementation of the protocol. The same day, the government hosted a nationally televised program for healthcare professionals, outlining the recommendations on the use of the protocols to treat COVID-19.
Then the country formed what they called “medical brigades,” which went house to house — especially in underserved areas of the country — to begin early treatment for those requiring the out-patient protocol medications.
The results? In a word — stunning.
The study researchers wrote: “The case fatality rate for COVID-19 in Honduras dropped below the lower control limit 9 days after implementation of an in-patient multidrug protocol, from an average of 9.33% case fatality rate to 5.01%. The Honduran COVID-19 case fatality rate again dropped below the 5.01% control chart limit 17 days after implementation of an out-patient multidrug protocol, to an average of 2.97%, suggesting statistically significant anomalies. No control limit anomalies were seen during the same period in neighboring Mexico.”
“These results really demonstrate what you can achieve by taking a simple, common sense approach to treating an emerging disease,” said Dr. Paul Marik. “Imagine what could have happened if we had done the same in the United States?”
As this article is being written — two years after the start of the pandemic — the United States has just put forth its first standard of care for COVID-19 outpatients that includes two understudied, expensive, difficult to obtain and possibly dangerous drugs from Merck and Pfizer. Other than that, the policy is “Wait until your lips turn blue and you cannot breathe. Then come into the hospital.” This is NOT a standard of care. It’s a recipe for catastrophe.
It is now estimated by many leading critical care physicians and COVID-19 researchers that, had this country developed and promoted early treatment for COVID-19, over 500,000 Americans would still be alive today. Half a million people. Gone, unnecessarily. Not to mention the signal that would have been sent to other countries.
Our country’s response to COVID offers another master class: How to Put Profits Before People 101.
Source: Honduras’ Master Class: Treating COVID Early 101