Four days ago, a paper was published at this link.
It was published in The Journal of Antibiotics, which is part of the Nature Publishing Group (NPG); a publisher that has traditionally been highly respected in the field of science.
The paper is entitled “Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model“
Here is the full reference:
Uematsu, T., Takano, T., Matsui, H., Kobayashi, N., Ōmura, S., & Hanaki, H. (2023). Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model. The Journal of Antibiotics. doi:10.1038/s41429-023-00623-0
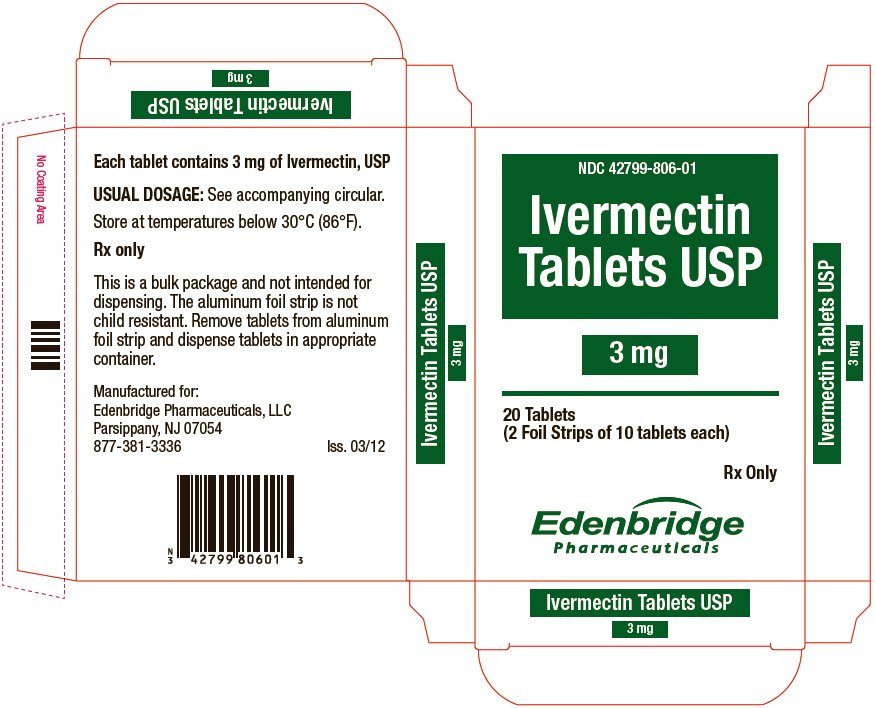
Ivermectin, a drug intended for use in humans…
Note that the Syrian hamster that is referred to in the study is the most commonly used animal model for pre-clinical research of COVID-19.
Here is the most important take-home message from the paper (I’ve bolded what I thought were the key points)…
“In conclusion, we demonstrate the efficacy of prophylactic administration of ivermectin in a hamster model of SARS-CoV-2 infection. Ivermectin and its derivatives may represent an effective therapeutic option for COVID-19; however, further in vitro and in vivo analyses are required to determine the optimal dose and method of administration of ivermectin. High quality clinical trials are required to fully elucidate the mechanism of action of ivermectin and validate the potential of ivermectin as a therapeutic option for the prevention and treatment of COVID-19.”
First, I appreciate that these scientists went back to the starting point and ran a good-quality pre-clinical study. The results add further strength to the pre-clinical foundation supporting the concept of assessing ivermectin and/or its derivatives as repurposed drugs in people in the context of COVID-19. We are supposed to follow the weight of the scientific evidence and the weight of the pre-clinical evidence in the literature justifies human clinical trials.
But, there have been quite a few human clinical trials performed in this area. So, why is there still debate? The authors of this paper hit upon what was likely their most important conclusion of all; that high quality clinical trials of ivermectin or its derivatives are required.
Clinical trials, especially those that concluded no benefit of ivermectin in the context of COVID-19, are generally not of the highest quality scientific designs. Appallingly, studies that countered the idea that ivermectin could benefit people with COVID-19 (or even prevent it) often had fatal flaws. So bad were some of the experimental designs that one might even be justified in questioning if there was an intent to bias the outcomes against ivermectin. This includes, but is not limited to things like:
- Running trials in countries where ivermectin was readily available and being used as an over-the-counter medicine, but not accounting for this in control groups. So, a known treatment regimen with ivermectin was likely being compared to an undefined treatment regimen with ivermectin, at least to some degree.
- Failing to confirm via serological testing that treatment groups were taking ivermectin as prescribed and confirming the absence of ivermectin in control groups.
- Enrolling patients at a stage of disease severity at which ivermectin (any drug for that matter) does not perform as well; its optimal usage is prophylactically (i.e., to prevent disease) or in the early stages of disease, not when it is so bad that a person must go to a hospital.
- Using sub-optimal dosing regimens.
- Etc.
So, we are still apparently in need of HIGH QUALITY human clinical trials to optimize the use of ivermectin in people.
Remarkably, this statement made by the authors…
“These results indicate that ivermectin may have efficacy in reducing the development and severity of COVID-19“
…is the best that anyone could ever try to conclude for the COVID-19 shots after an avalanche of data. And even this is now in question, as emerging relatively transparent public health data in a growing number of countries suggests that the accusation of this being a “pandemic of the unvaccinated” was based on highly unreliable and unethically manipulated data. Worse, when the unethical data manipulations are removed from the equation, public health data suggest that people who received multiple COVID-19 shots, especially boosters, are likely more susceptible to getting COVID-19 and are more prone to greater severity of disease.
As a scientist, I have been appalled at the unacceptably low quality of many of the human clinical trials that have been conducted over the past three years. Many have been so poorly designed that their results are untrustworthy. This includes studies on repurposed drugs for COVID-19, masking to prevent infections, safety and efficacy of COVID-19 ‘vaccines’, new drugs to treat COVID-19, and others.
As a pre-clinical scientist I have to admit that I was largely blissfully unaware of the poor state of clinical experimentation in the world. After all, I was focused on early studies where ideas are generated and initially tested and optimized for potential downstream use in people. I was highly successful in my quiet and safe world of early-phase research studies. But, over the past three years I pulled my head out of the proverbial sand to dig deep into the COVID-19 clinical trial literature. Frankly, the state of so-called ‘advanced’ clinical research is embarrassing for the most part. If my research team conducted pre-clinical research like most clinical trials have been performed in past few years, we would have great difficulty publishing our findings, and rightly so.
Experimental designs for many clinical trials don’t come close to meeting my standards for pre-clinical studies, which cost about three orders of magnitude less money. I am proud of my research team. We make the design of our experiments a top priority. We endeavour to ensure that all relevant controls are incorporated. We do our best to eliminate confounding variables. We maximize the amount and quality of data that are generated so the research will be as cost-effective and informative as possible, while minimizing the use of animal models. Most importantly, even though we design and test novel treatment strategies, we remain diligent in looking for evidence of potential off-target effects. In fact, I often teach my students the ‘tricks’ used in research to make new treatments seem more effective and safe than they are, and then encourage everyone to avoid doing this. My research team has developed a reputation for conducting robust research with integrity.
I suspect that most members of the public do not realize how expensive clinical trials are. Nor do many understand how many taxpayer dollars are invested into all stages of research, but especially the early ones. Late-stage research is so expensive (millions of dollars) that it can usually only be supported by entities with commercial interests. These commercial entities have governing boards for whom making money for their investors is an essential priority for the health of their business. But, even in advanced clinical stages of research, academics are also usually involved. And their salaries and academic institutions are funded by the public.
So, the public has a vested interest in knowing why so many clinical trials have failed to meet standards that are the norm for vastly cheaper pre-clinical studies. Why are animal studies often run to a higher standard than human experimentation? At the end of the day, I would contend that the responsibility for this rests with our public health regulatory agencies. On paper they are to serve the best interests of the public, but their budgets are primarily funded by the commercial entities that they are asked to regulate. Regulators at these agencies are tasked with hashing out the designs of clinical trials with the people conducting them. Only once these are approved can clinical trials commence. So, I would argue that public health regulatory agencies have been failing the public and wasting A LOT of their money in the process. Take the masking literature as an example. One thing that most comprehensive analyses of this area of science have concluded is that the quality of most trials has been low and that high quality future studies are needed.
The public must demand better from their health regulatory agencies!
There needs to be a comprehensive and objective review of their funding structures as it relates to the potential for conflicts of interest. And if they cannot do their jobs properly, we need to re-staff them with scientists of integrity, including those with pre-clinical experience, and then provide these new hires with a level of job security that would over-ride any potential consequences for making rulings improperly supported narratives.
How does it make you feel to be three years into a declared pandemic in which study after study after study has been conducted on ivermectin, masks, COVID-19 shots, etc., only to keep hearing something to the effect that the next multimillion-dollar study should be a properly designed one?
Shouldn’t the very first clinical trial and any subsequent to that be designed in a way that the results would be considered trustworthy? It seems to me that current methods to design clinical trials are, for the most part, fundamentally flawed and in urgent need of being revamped.
The scientific method is based on identifying a problem, posing a probing question, and then developing a probing hypothesis. The authors of the paper highlighted in this article identified that high quality clinical trials are needed to investigate the potential benefits of ivermectin in the context of COVID-19.
My hypothesis is this:
Future high quality clinical trials of the Nobel prize-earning drug that has been promoted for use in millions of people worldwide over a very long period of time with an incredible safety profile (also known as ivermectin) will be proven to have had the potential to have saved lives and reduced the morbidity of millions of people over the past three years.
Anyone putting forth a hypothesis is not promoting ‘misinformation’. Rather, they are helping to inform an area in need of research. Am I wrong? For the naysayers, I say run a proper, objective, well-designed, extensively vetted trial to definitively prove or disprove this hypothesis. I will follow the science, but only if it is of adequate quality.
**Source: Pre-Clinical Support of High Quality Ivermectin Studies
