COVID-19 is no longer classed as a global health emergency by the World Health Organization, but scientists are still working hard to understand more about the virus and its impact – including how the coronavirus affects the body and leads to death.
A new analysis suggests that a high percentage of people who required help from a ventilator due to a COVID-19 infection also developed secondary bacterial pneumonia. This pneumonia was responsible for a higher mortality rate than the COVID-19 infection.
So while COVID-19 may have put these patients in the hospital, it was actually an infection brought on by the use of a mechanical ventilator that was more likely to be the cause of death when this infection didn’t respond to treatment.
“Our study highlights the importance of preventing, looking for, and aggressively treating secondary bacterial pneumonia in critically ill patients with severe pneumonia, including those with COVID-19,” says Benjamin Singer, a pulmonologist at Northwestern University in Illinois.
The team looked at records for 585 people admitted to the intensive care unit (ICU) at Northwestern Memorial Hospital, also in Illinois. They all had severe pneumonia and/or respiratory failure, and 190 had COVID-19.
Using a machine learning approach to crunch through the data, the researchers grouped patients based on their condition and the amount of time they spent in intensive care.
The findings refute the idea that a cytokine storm following COVID-19 – an overwhelming inflammation response causing organ failure – was responsible for a significant number of deaths. There was no evidence of multi-organ failure in the patients studied.
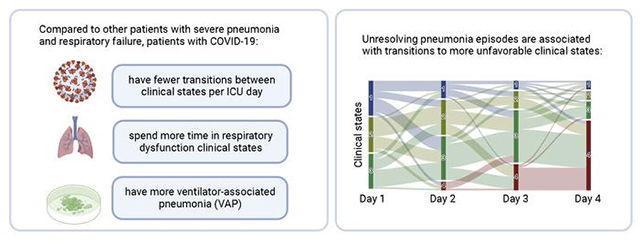
Instead, COVID-19 patients were more likely to develop ventilator-associated pneumonia (VAP) and for longer periods. Cases where VAP didn’t respond to treatment were significant in terms of the overall mortality rates in the study.
“Those who were cured of their secondary pneumonia were likely to live, while those whose pneumonia did not resolve were more likely to die,” says Singer.
“Our data suggested that the mortality related to the virus itself is relatively low, but other things that happen during the ICU stay, like secondary bacterial pneumonia, offset that.”
These results suggest that ICU outcomes could be improved if there were better strategies to diagnose and treat VAP episodes – something that the researchers say needs to be addressed in the future.
It’s worth bearing in mind that if a patient’s requirement for a ventilator to treat COVID-19 complications leads to VAP, this doesn’t imply that a COVID-19 infection is less dangerous, nor does it decrease the number of COVID-19 fatalities.
As the authors write in their paper, “The relatively long length of stay among patients with COVID-19 is primarily due to prolonged respiratory failure, placing them at higher risk of VAP.”
But the findings highlight a need for further study and to be cautious when making assumptions about the cause of death in COVID-19 cases. A detailed molecular analysis from the same study should reveal more about what makes the difference between recovering or not from VAP.
It’s also another example of how machine learning artificial intelligence can process vast amounts of data and spot patterns beyond us mere humans – whether it’s analyzing proteins or advancing mathematics.
“The application of machine learning and artificial intelligence to clinical data can be used to develop better ways to treat diseases like COVID-19 and to assist ICU physicians managing these patients,” says Catherine Gao, also a pulmonologist at Northwestern.
The research has been published in the Journal of Clinical Investigation.
