BREAKING! U.S. Study Finds That SARS-CoV-2 Infections And mRNA Jabs Alter DNA Methylation States Of Immune Cells And Epigenetic Clocks Of Humans!
SARS-CoV-2 Epigenetics: A new study led by researchers from Weill Cornell Medicine-New York that also involved scientists from Icahn School of Medicine at Mount Sinai-New York, , Comite Center for Precision Medicine & Health-New York, Yale University School of Medicine-Connecticut, VA Connecticut Healthcare System and TruDiagnostic, Lexington-Kentucky has alarmingly found that both SARS-CoV-2 infections and COVID-19 mRNA jabs causes altered DNA methylation states of immune cells and also the epigenetic clocks in humans!
This alarmingly implies that both routes cause a dysfunctional immune state in all human either infected with the SARS-CoV-2 virus or have been given the mRNA jabs.Urgent further studies are warranted to validate these findings and for all concerned to take remedial actions as soon a possible!
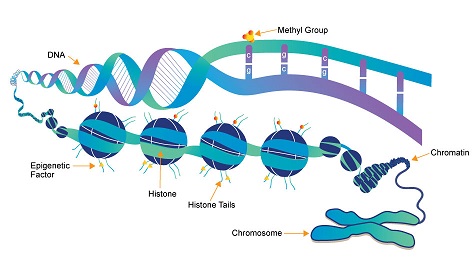
The human host epigenetic landscape rapidly changes during SARS-CoV-2 infection, and evidence suggest that severe COVID-19 is associated with durable scars to the epigenome.
Importantly, aberrant DNA methylation changes in immune cells and alterations to epigenetic clocks in blood relate to severe COVID-19.
An epigenetic clock is a biochemical test that can be used to measure age. The test is based on DNA methylation levels, measuring the accumulation of methyl groups to one’s DNA molecules.
To date however, a longitudinal assessment of DNA methylation states and epigenetic clocks in blood from healthy individuals prior to and following test-confirmed non-hospitalized COVID-19 has not been performed.
Furthermore, the impact of mRNA COVID-19 vaccines upon the host epigenome remains understudied.
This is the first documented study to examine DNA methylation states in the blood of 21 participants prior to and following test-confirmed COVID-19 diagnosis at a median time frame of 8.35 weeks; 756 CpGs were identified as differentially methylated following COVID-19 diagnosis in blood at an FDR adjusted p-value
Principal component-based epigenetic clock estimates of PhenoAge and GrimAge significantly increased in individuals over 50 following infection by an average of 2.1 and 0.84 years.
In contrast, PCPhenoAge significantly decreased in individuals fewer than 50 following infection by an average of 2.06 years.
Shockingly, this observed divergence in epigenetic clocks following COVID-19 was related to age and immune cell-type compositional changes in CD4+ T cells, B cells, granulocytes, plasmablasts, exhausted T cells, and naïve T cells.
Further complementary longitudinal epigenetic clock analyses of 36 participants prior to and following Pfizer and Moderna mRNA-based COVID-19 vaccination revealed that vaccination significantly reduced principal component-based Horvath epigenetic clock estimates in people over 50 by an average of 3.91 years for those who received Moderna!
This reduction in epigenetic clock estimates was significantly related to chronological age and immune cell-type compositional changes in B cells and plasmablasts pre- and post-vaccination.
The www.thailandmedical.news/articles/coronavirus”>SARS-CoV-2 Epigenetics study findings also suggest the potential utility of epigenetic clocks as a biomarker of COVID-19 vaccine responses. Future research will need to unravel the significance and durability of short-term changes in epigenetic age related to COVID-19 exposure and mRNA vaccination.
The study findings were published in the peer reviewed journal: Frontiers In Genetics. https://www.frontiersin.org/articles/10.3389/fgene.2022.819749/full
For layman who are not well versed with various biological terms, the study findings basically states that both SARS-CoV-2 infections and COVID-19 mRNA jabs will cause epigenetic changes to important genes in your immune system and that you will end up with a dysfunctional immune system and also possibly a reduced life span to a certain degree!
This is the first study to examined whether SARS-CoV-2 infection and mRNA COVID-19 vaccination impacted DNA methylation states and epigenetic clocks in healthy individuals in the short term.
The study findings revealed that significant differences in DNA methylation in blood associate with SARS-CoV-2 infection at 756 CpG sites, suggesting an immune cell-based epigenetic signature of COVID-19 may derive from aberrant DNA methylation states related to immune dysfunction induced by COVID-19.
The study findings support epigenetic findings from other groups that have reported distinct DNA methylation states in blood as a potential biomarker of COVID-19.
https://link.springer.com/article/10.1186/s13148-021-01102-9
https://pubmed.ncbi.nlm.nih.gov/33867313/
https://pubmed.ncbi.nlm.nih.gov/34185889/
The epigenetic clock findings reveal an age-related impact of epigenetic age increase associated with natural SARS-CoV-2 infection on the PCPhenoAge epigenetic clock and mortality risk estimate PCGrimAge in mild/moderate cases. Whether the extent and durability of this perturbation to these two epigenetic clock estimates is related to long COVID-19 or long-term aging outcomes remain an intriguing area for further investigation.
The study findings support a recent cross-sectional human DNA methylation study of COVID-19 that reported DNA methylation patterns of COVID-19 convalescents compared to uninfected controls. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/ppcovidwho-294985
The study also provides the first examination of longitudinal DNA methylation changes in the blood of healthy participants prior to and following test-confirmed mild/moderate COVID-19.
The study team observed blood-based DNA methylation changes associated with COVID-19 exposure in healthy participants ranging in age with 756 differentially methylated CpGs identified. Among the COVID-19 differentially methylated loci detected in blood, they observed hypermethylation related to the caspase recruitment domain family member 14 (CARD14) gene. This gene encodes a protein that has been shown to interact with BCL10 that functions as a positive regulator of cell apoptosis and NF-kappa-B activation.
CARD14 also may play a role in protecting cells against apoptosis. The study team observed that the percent change in DNA methylation inferred immune cell type proportion for CD8 T cells for participants following COVID-19 exposure significantly associated with the DNA methylation percent change related to CARD14.
This suggests that a subset of DNA methylation changes related to COVID-19 exposure were due to cell type compositional changes. Notably, the team also observed the differentially methylated CpGs associated with COVID-19 were enriched in transcriptional gene sets identified from published SARS-CoV-2 human, animal model, and in vitro infection studies. https://pubmed.ncbi.nlm.nih.gov/27141961/
The study findings suggest that DNA methylation changes associated with COVID-19 likely participate in the regulation and modulation of host gene expression from infection. Together, this first set of findings support the notion that distinct host DNA methylation states in circulating immune cells serves as a COVID-19 specific epigenetic signature. The durability of this COVID-19 epigenetic signature remains a key question for future study.
The study findings also contradict previous studies and suggests that specific epigenetic clocks may be altered by COVID-19 based on age.
The study team utilized a more powerful longitudinal study design of individuals prior to and following test-confirmed COVID-19 and applied a novel principal component-based assessment of epigenetic clocks that mitigates issues with reliability in standard epigenetic clock algorithms.
The team observed a divergence in the epigenetic clock estimate PCPhenoAge and epigenetic clock mortality algorithm PCGrimAge based on age in individuals following COVID-19. Slight epigenetic age acceleration in the short term appeared in those individuals over 50 years of age that were infected with SARS-CoV-2. In contrast, epigenetic age appeared to reduce in those individuals less than 50 years of age following COVID-19. PCPhenoAge and PCGrimAge are among the strongest epigenetic predictors of mortality risk.
The study findings support the critical role of age as a COVID-19 risk factor and suggest that specific epigenetic clocks can capture an age-dependent perturbation to epigenetic clocks following COVID-19.
Prior multi-omic analysis has shown that the Levine clock accelerates with cellular senescence and mitochondrial dysfunction.
https://pubmed.ncbi.nlm.nih.gov/32930491/
Past studies of epigenetic clocks in COVID-19 utilized different sets of clocks, which may explain their conflicting results.
https://pubmed.ncbi.nlm.nih.gov/34200325/
https://jlb.onlinelibrary.wiley.com/doi/10.1002/JLB.5HI0720-466R
https://pubmed.ncbi.nlm.nih.gov/34502212/
A plausible interpretation of PCPhenoAge/PCGrimAge results after infection is an age-related signal of both immunosenescence and inflammaging. Once the immune system is activated in younger individuals by SARS-CoV-2 infection, they look younger by the epigenetic clock due to a robust activation of the immune response that reflects in younger individuals (not that they are actually becoming younger). In older individuals, activation of non-specific inflammatory pathways after SARS-CoV-2 infection appears to increase the epigenetic age because of the activation of pathways that overlap are similar to inflammaging. An alternative interpretation for divergence in epigenetic age based on age during SARS-CoV-2 infection might involve the biological process of hormesis: moderate stressors can improve health by causing a compensatory response. COVID-19 might serve as a hormetic stress in non-hospitalized younger individuals, while it serves as a toxic stressor in older adults or any severe case.
It has been found that aging drives immunosenescence with implications for a decline in adaptive immunity resulting in reduced vaccine responses and vaccine durability in older adults. The age-related decline in immune function including reduced thymic output of naïve T cells and dampened B cell generation has notably led to decreased vaccine efficacy in older individuals.
https://pubmed.ncbi.nlm.nih.gov/33320183/
Building evidence for COVID-19 indicate a declined humoral and cellular immune response in older individuals.
https://pubmed.ncbi.nlm.nih.gov/34192737/
https://pubmed.ncbi.nlm.nih.gov/34614326/
Unfortunately, failure to achieve a protected or durable response after vaccination is poorly understood despite occurring commonly among many elderly individuals.
The epigenetic clock data following mRNA COVID-19 vaccination revealed an age-related decrease in epigenetic age following vaccination. The study findings also revealed that the change in epigenetic age following vaccination was specifically related to immune cell type compositional changes in the percentage of B cells, plasmablasts, and granulocytes. These findings support work showing that SARS-CoV-2 mRNA vaccines induce persistent germinal center B cell response that enables robust humoral immunity. https://pubmed.ncbi.nlm.nih.gov/34182569/
The study findings do not provide any insights into the particular impact of the mRNA lipid nanoparticle compared to the expressed spike protein upon different epigenetic clocks. These compelling findings suggest that epigenetic profiles and specifically epigenetic clock estimates may provide insights into individual and age-related humoral immune responses to COVID-19 vaccination.
Recent studies examining T cell exhaustion after recovery from chronic infection in humans has found that epigenetic scars of CD8+ T cell exhaustion persists in humans, suggesting indelible imprints on the host immune cell epigenome from viral infection. https://pubmed.ncbi.nlm.nih.gov/34312547/
The hypothesis of a persistent epigenetic dysregulation of host immune cells contributing to long COVID-19 remains unclear. Whether durable changes to epigenetic clocks are reflected by epigenetic scars of particular immune cell types and relate to long COVID-19 is a compelling hypothesis to pursue.
The study findings highlight the benefits of the study team’s computational solution using principal components for calculating PC-based epigenetic clocks for longitudinal studies. Utilizing standard epigenetic clock estimates, the study team observed variation up to 9 years in participants pre- and post-timepoint samples epigenetic age estimates for all clocks that lead to non-significant results. While the application of PC-based epigenetic clocks pulled out a biological signal suggesting that mild/moderate COVID-19 from SARS-CoV-2 infection and mRNA vaccination impacted epigenetic clocks, the biological mechanisms that influence detrimental or beneficial changes in epigenetic clocks remains unclear.
The methylation dataset on vaccines was obtained at a median post second dose of around 2 months. Based on data showing durability of vaccine responses out to 6 months post-vaccination, our DNA methylation data were captured during an effective post-vaccine time frame window. https://pubmed.ncbi.nlm.nih.gov/33822494/
Longitudinal epigenetic studies are considered the gold standard study design to mitigate interindividual variation in DNA methylation patterns and track environmental and pathogen-induced changes to the epigenome. Hence, the study team’s assessment of longitudinal DNA methylation of 21 participants provides a discovery dataset for examining the short-term impacts of COVID-19 upon the host immune cell epigenome and impact on epigenetic clock estimates.
The longitudinal COVID-19 DNA methylation dataset consisted of healthy participants that ranged across the lifespan from 18 to 73 years of age. Moreover, the collection of DNA methylation data following test-confirmed COVID-19 exposure occurred within a short-term time frame of a 6-months window and occurred early during the COVID-19 pandemic reflecting infection with a less evolved, less contagious, and potentially less severe SARS-CoV-2 virus than recent variants such as the Delta variant.
Hence, the study findings are limited by these potential factors. These longitudinal findings need to be confirmed in a larger sample size, across diverse regions and genotypes, among individuals across the lifespan, in people infected with emerging SARS-CoV-2 variants, and across COVID-19 severities including those individuals who recover and suffer from long-lasting symptoms termed post-COVID.
For more on epigenetic effects of SARS-CoV-2 infections and mRNA jabs, keep on logging to Thailand Medical News.
