Per a recent Medscape article, many physicians claim to experience emotional damage, financial losses, and are less likely to trust patients due to medical malpractice lawsuits.
November 4, 2023: With medical malpractice being among the top causes of death, many Americans (including myself) have witnessed the catastrophic injury or loss of a loved one due to misdiagnoses, harmful treatments, and high-risk and/or unnecessary treatments, procedures, or surgeries that were administered to a patient without consent, informed or otherwise.
When catastrophic medical injuries occur, victims and their loved ones often contemplate whether or not to sue the hospital or healthcare providers responsible for the injury done to themselves or a loved one that was the result of gross medical negligence or willful ignorance.
Medscape conducted a survey of over 3,000 U.S. physicians between May 5, 2023 – July 5, 2023, across 29 specialties to assess the risk for malpractice lawsuits and how they perceive their patients. The answers from physicians regarding their experience with medical malpractice and how it changed their perception of patients are shocking.
While the negative consequences of medical malpractice to a patient and their family may result in permanent disfigurement, disability, disease, or death, thereby causing traumatic emotional damage and often times massive financial losses, the relative ‘negative consequences’ to the healthcare providers is minimal.
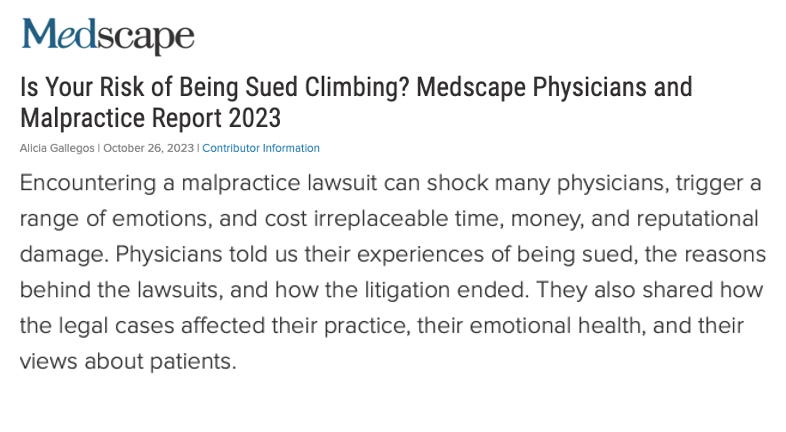
In the recent Medscape article, the author frames physicians as the victims in medical malpractice cases, claiming;
Encountering a malpractice lawsuit can shock many physicians, trigger a range of emotions, and cost irreplaceable time, money and reputational damage…They also shared how the legal cases affected their practice, their emotional health, and other views about their patients.”
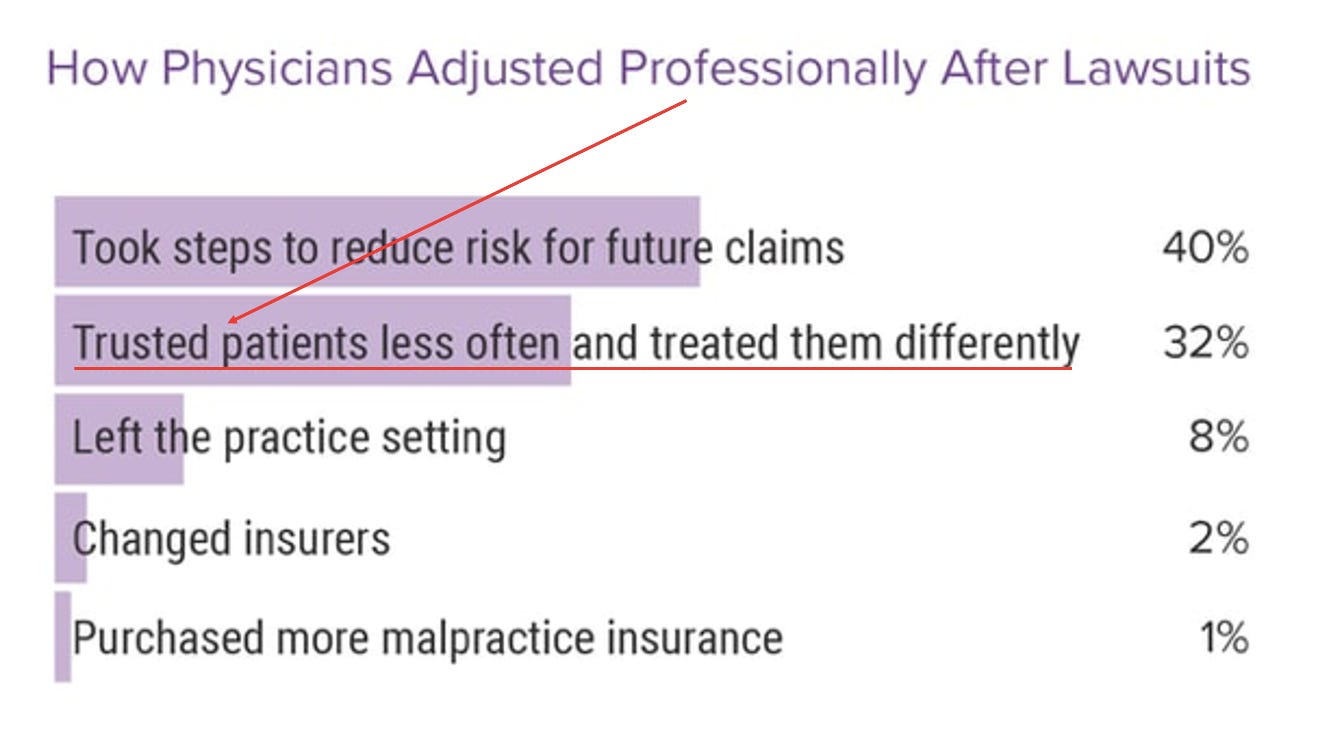
When physicians were asked how they ‘professionally adjusted their practice after a lawsuit,’ 32% responded that they ‘trusted patients less’ and ‘treated them differently.’
“I find this claim to be a bit ironic because the majority of patients are told to simply “trust the science” or ‘trust the medical expert,’ but if the medical expert and their trusted science harms us or a loved one, we’re now the ones that are untrustworthy!?” – Karen Kingston
Risk factors that are typically used to determine a patient’s risk for negative clinical outcomes such as injury, disability, disease, and death, include examples such as the patient’s age, weight, co-morbid conditions, and diet and exercise habits. I didn’t realize that ‘patient trustworthiness’ was a risk factor for suffering disfigurement, disability or death after undergoing a medical treatment or procedure. (But then again, the entire globe just locked down due to a ‘virus’ that’s symptoms included ‘no symptoms at all.’)
It appears that approximately 8% of physicians who are sued seem to truly do experience significant financial loss or emotional trauma, as they ended up leaving the practice setting after a lawsuit.
While 40% of physicians reported that they took steps to reduce the risk for future malpractice claims, the reality is that physicians strongly supported legal tactics that would ensure medical malpractice cases would rarely if ever be able to be brought to court.
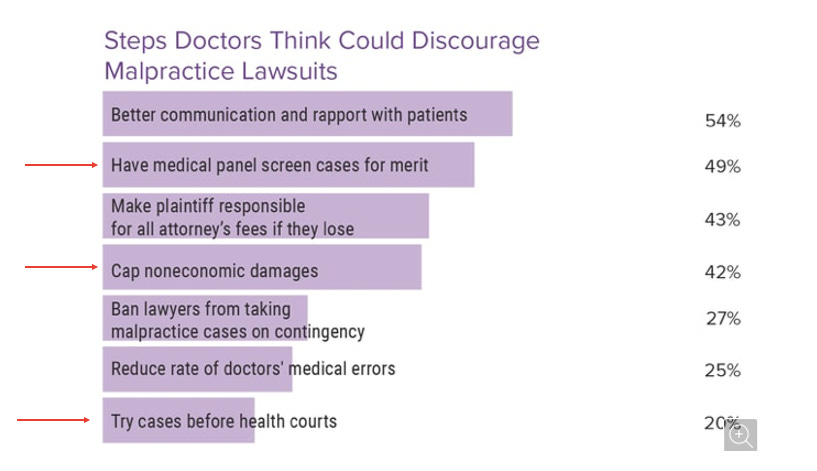
In order to discourage patients from suing doctors for malpractice, 49% of physicians recommended that all medical malpractice lawsuits should be heard in front of a panel of their peers before a judge would even be able to review a patient’s claim for medical malpractice.
20% of physicians recommended that medical malpractice lawsuits be tried in health courts. (I assume these health courts would be comprised of healthcare workers and industry experts as the judges, juries, and prosecutors).
I call both of the above tactics the, “Who’s Going to Give a Police Officer a Speeding Ticket?” strategy. The answer is ‘NO ONE.”
It is highly unlikely that a panel of doctors is going to throw one of their peers under the bus at the risk of that peer being on a future medical malpractice panel for a lawsuit that he or she is named as a defendant in.
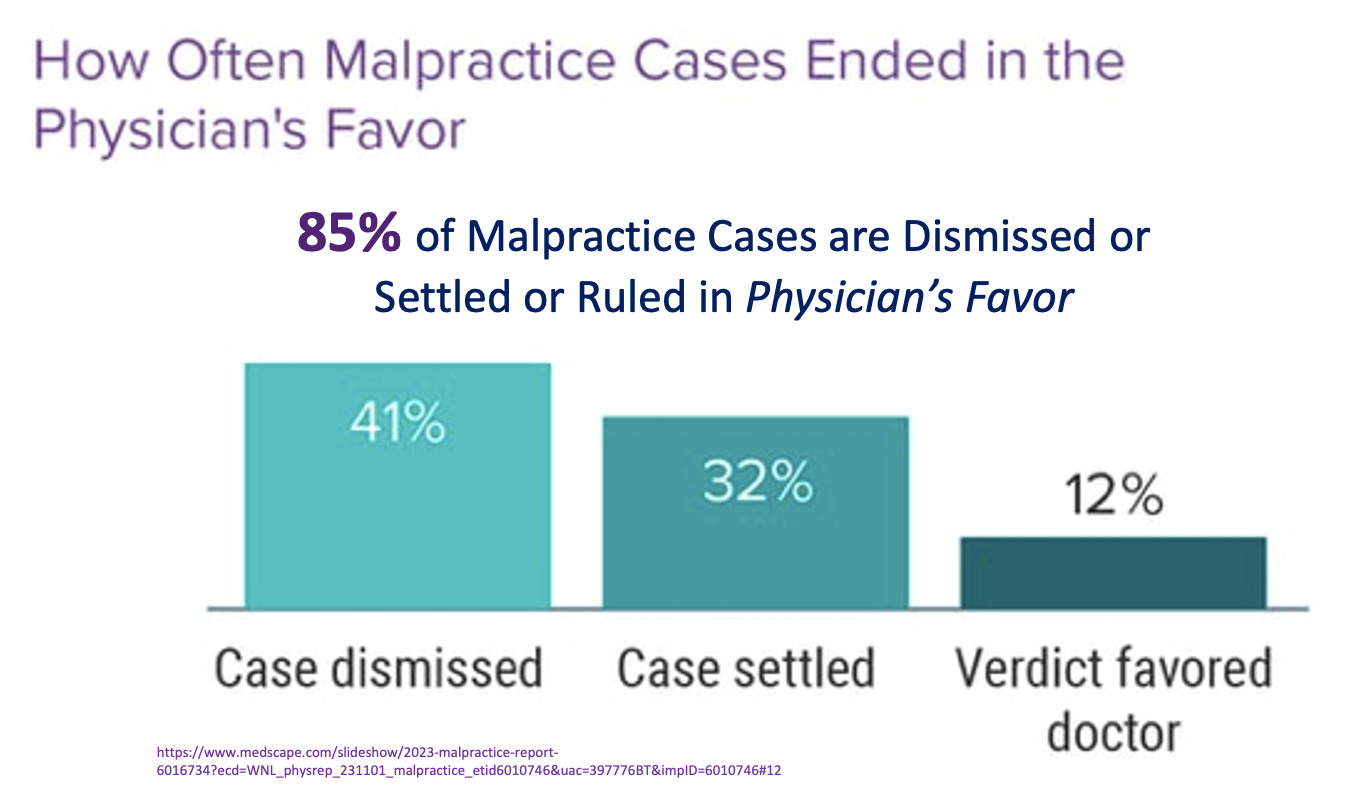
Although 55% of physicians reported that they have been named as a defendant or co-defendant in one or more medical malpractice lawsuits, doctors rarely, if ever suffer major financial loss after losing a medical malpractice case. One of the reasons is that they have malpractice insurance to cover the claims and the other reason is that 85% of malpractice cases end in the favor of the physician.
Not surprisingly, when victims bring forth a medical malpractice case against their healthcare provider, 41% are dismissed, and 44% are settled or ruled in favor of the physician(s).
According to the MedScape survey data, patient victims have a 15% chance (or less of winning a case.)
In 36% of cases that favored the plaintiff (patients), the plaintiff was awarded a financial amount ranging between $0 and $100,000.
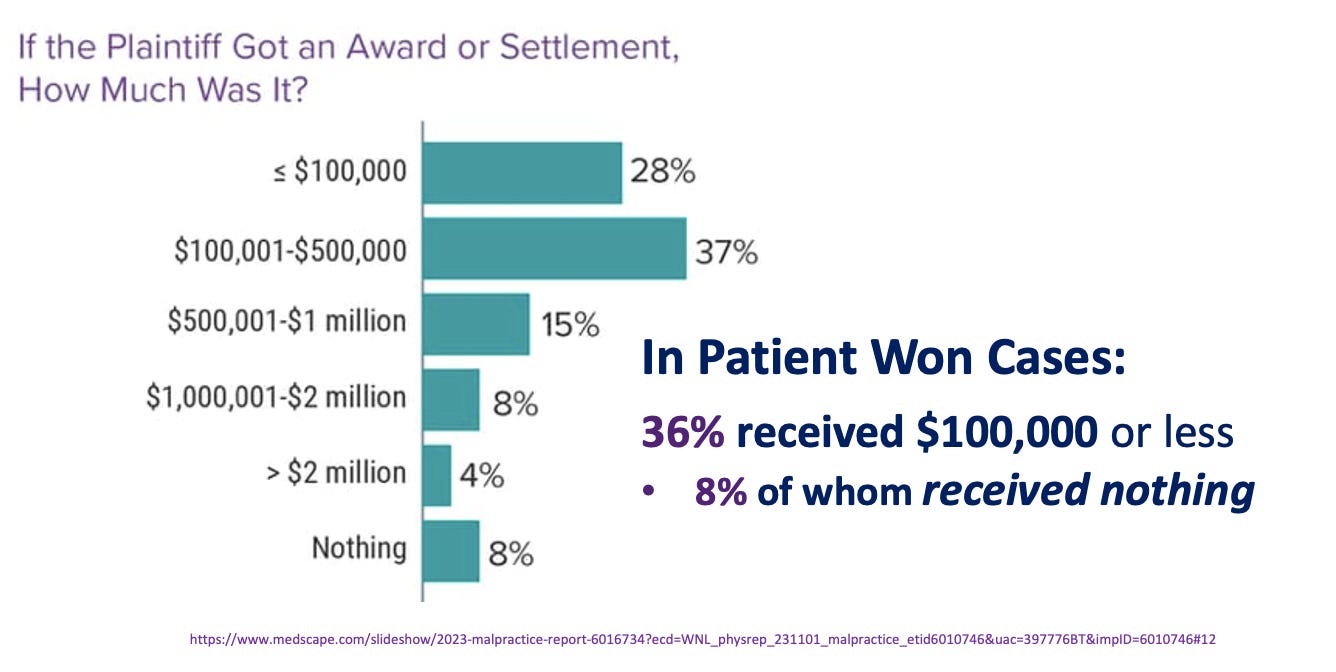
While $100,00 may seem like a large award, when medical negligence or malpractice results in permanent disability, disfigurement, or death of a patient, the victim and his/her family are often left financially, mentally, and emotionally devastated.
In my opinion, this Medscape survey and article is pandering to physicians and healthcare providers making them out to be the most virtuous, competent, and impeccable group of professionals who should be able to create their own laws and standards for themselves, regardless of any irreparable harm they may cause their patients or their loved ones, even when it’s intentional.
Source: Are Physicians the ‘Real Victims’ of Medical Malpractice Lawsuits?
