Michael Palmer MD and Sucharit Bhakdi MD
Summary
This expert statement makes the case that
- the WHO’s act of declaring COVID-19 a “pandemic” was unjustified;
- COVID-19 poses a negligible risk of permanent harm to otherwise healthy persons, particularly those of young age;
- no empirical evidence exists to support the use of masks, social distancing, or lock-downs to prevent the spread of COVID;
- empirical evidence does exist to show that healthy people do not infect others with COVID;
- lock-downs, school closures and other scientifically baseless ‘pandemic control measures’ have devastating effects on the mental health of our children.
Measures such as lock-downs, mask mandates, and school closures are therefore unsupportable and should be revoked.
1. The misconception of the “COVID-19 emergency”
The WHO issued its declaration of a “pandemic” on March 11th, 2020. Considering that less than two weeks before that date the number of “cases” reported worldwide had been only 80,000 [1], this declaration was strangely premature. However, this low case number is not the only thing that was amiss with this “emergency.”
1.1. The WHO’s criteria for calling a “pandemic” are flawed
British Medical Journal editor Peter Doshi has pointed out that, shortly before Swine Flu was declared a “pandemic” in 2009, the WHO had redefined its criteria for making such a declaration [2]. According to Doshi, as of 2003 the now defunct WHO Pandemic Preparedness homepage had contained the following statement:
An influenza pandemic occurs when a new influenza virus appears against which the human population has no immunity, resulting in several simultaneous epidemics worldwide with enormous numbers of deaths and illness.
A definition that includes “enormous numbers of death and illness” is certainly in keeping with the general understanding of the term “pandemic,” considering that it is commonly used in connection with the “Black Death” of the Middle Ages or with the Spanish Flu of 1918. However, the WHO’s revised definition from 2009 does not contain any reference to deaths or disease severity. As of that year, the same WHO web page merely stated:
An influenza pandemic may occur when a new influenza virus appears against which the human population has no immunity.
Nor do death or clinical disease severity receive any mention in the more detailed definition given by the WHO’s 2009 guidance document on influenza epidemics, which is currently still available [3]. Accordingly, pursuant to these guidelines, any new strain of influenza could be declared a “pandemic,” whether or not it results in significant surplus mortality and morbidity.
Considering the far-reaching and detrimental consequences for commerce, international travel etc., it should go without saying that declaring a pandemic is disproportionate and unjustified when the disease in question is merely widespread but not severe. Exactly this kind of malfeasance, however, has occurred in the case of COVID-19: a pandemic was declared by the WHO, and subsequently by the governments of the world, without regard for clinical severity.
1.2. All-cause mortality soared only shortly after the declaration of the COVID-19 “pandemic,” not before
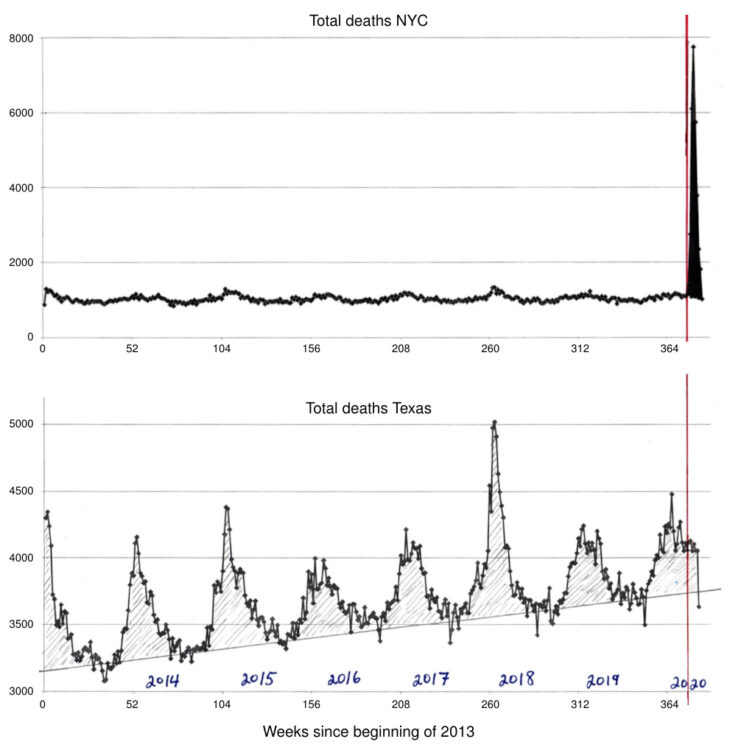
Rancourt has examined the correlation in time between the WHO’s declaration of the “pandemic” and all-cause mortality in various jurisdictions [4]. Immediately after the declaration, there occurred a sharp peak in all-cause mortality in some jurisdictions, but not in others; this discrepancy is illustrated in Figure 1 for New York City and Texas.
Common sense and historic precedents suggest that a deadly virus pandemic would not respect international or state borders. Furthermore, if the virus had indeed been both deadly and truly novel, the wave of deaths in New York should not have subsided within such a short time period as is apparent from Figure 1. Thus, as Rancourt convincingly argues, any peaks in mortality were most likely caused by government malfeasance, which led to consequences such as the rapid spread of the infection in senior homes. In the case of New York, this has led to the filing of criminal complaints against former governor Andrew Cuomo.
1.3. Mortality due to COVID-19 is very low except in the frail and elderly
In the vast majority of people (≥ 99.8% globally), an infection with SARS-CoV-2, the causative agent of COVID-19, is non-lethal [5–7]. It is typically a mild to moderately severe illness with a case fatality rate similar to that of influenza (see again Figure 1 for context). The relationship of COVID mortality with age is illustrated in Figure 2. Panel A very clearly shows that mortality is vanishingly small in the young and middle-aged. Moreover, even among the elderly, almost all fatal cases occur in people with co-morbidities. In Italy, the average age at the time of death was above 80 years, and only 0.8% of all fatal cases suffered from none of the 10 most common co-morbidities [8]. University of Hamburg forensic pathologist Prof. Klaus Püschel reviewed over 100 autopsies on patients at his institution whose deaths had been ascribed to COVID-19, and he concluded that not one of them had died due to COVID alone [9].
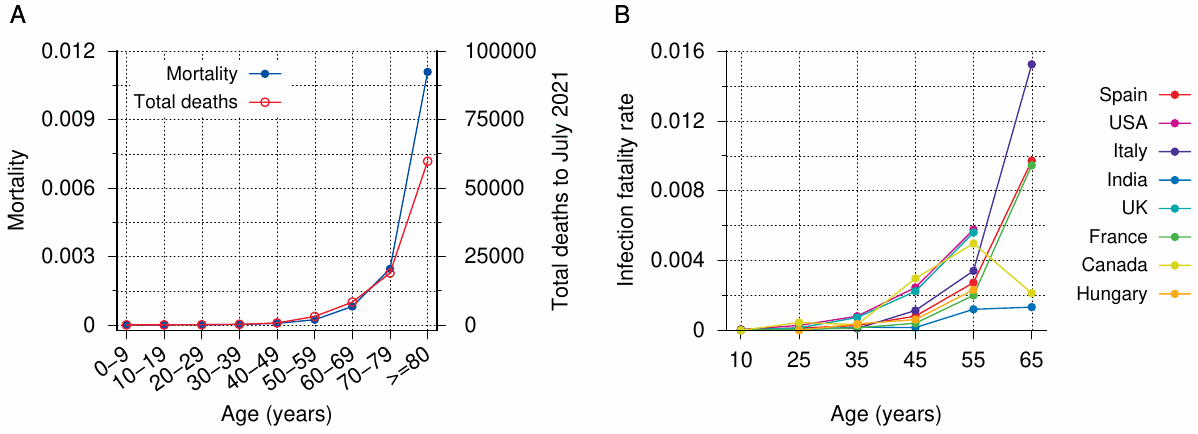
The collective findings can be summarized as follows: in otherwise healthy persons of all ages, COVID-19 poses a negligible risk of death or of severe disease with irreversible harm.
1.4. The misconception of the “pandemic” was implanted and perpetuated with inappropriate testing practices
From the very beginning, the number of COVID “cases” was artificially inflated by the inappropriate use of the PCR test. There are two key aspects to this misuse of the technique:
- the calibration of the method is inadequate; in particular, the number of amplification cycles is excessive;
- the application of the PCR test to healthy (“asymptomatic”) people, for example in connection with travel. This could not but generate a large number of false positive test results, which were then elevated to “cases.”
For further detail pertaining to this question, please refer to Prof. Ulrike Kämmerer’s separately submitted PCR expertise.
1.5. Flattening which curve?
When the first restrictions such as masks, “social distancing,” and lock-downs were imposed on the public, they were justified with the purported need to “flatten the curve,” that is, to slow down the spread of the virus so as to distribute clinically severe cases in time and thereby avoid the overload of hospitals with grave COVID cases. Media outlets such as the Canadian CBC propped up this narrative with invented stories about overflowing hospitals; see for example the fraudulent CBC story about triage of patients in the parking lot of the hospital in Steinbach, Manitoba—a reporter from another media outlet who investigate on-site found both the parking lot and the hallways of the hospital deserted [12].
In the real world, emergency room visits and hospital admissions declined after the declaration of the “pandemic;” this was consistently reported from various countries [13–17]. The reason for the decline was likely a general reluctance in the population to seek medical assistance, for fear of being infected with the supposedly deadly virus at the hospital. The decline was not offset by any proportional numbers of actual severe COVID cases. Thus, the need for “flattening the curve,” and with it that for imposing the very harsh and oppressive “emergency” measures, never existed.
2. On the necessity and effectiveness of the restrictions imposed by the governments
2.1. Do lock-downs and other restrictions reduce COVID mortality?
Reports like the one by Püschel (see Section 1.3) make it clear that COVID mortality statistics cannot be trusted. Püschel’s use of autopsies is of course the correct approach; in order to understand the seriousness of a novel pathogen, it would be essential to perform autopsies on as large a scale as possible. However, in general, autopsies were rarely performed and discouraged by the authorities worldwide. In their literature review entitled No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science, Salerno et al. observe [18]:
Despite the increasing number of published studies on COVID-19, in all the examined studies the lack of a well-defined pathophysiology of death among patients who died following COVID-19 infection is evident. Autopsy should be considered mandatory to define the exact cause of death … Only 7 papers reported histological investigations. Nevertheless, only two complete autopsies are described and the cause of death was listed as COVID-19 in only one of them.
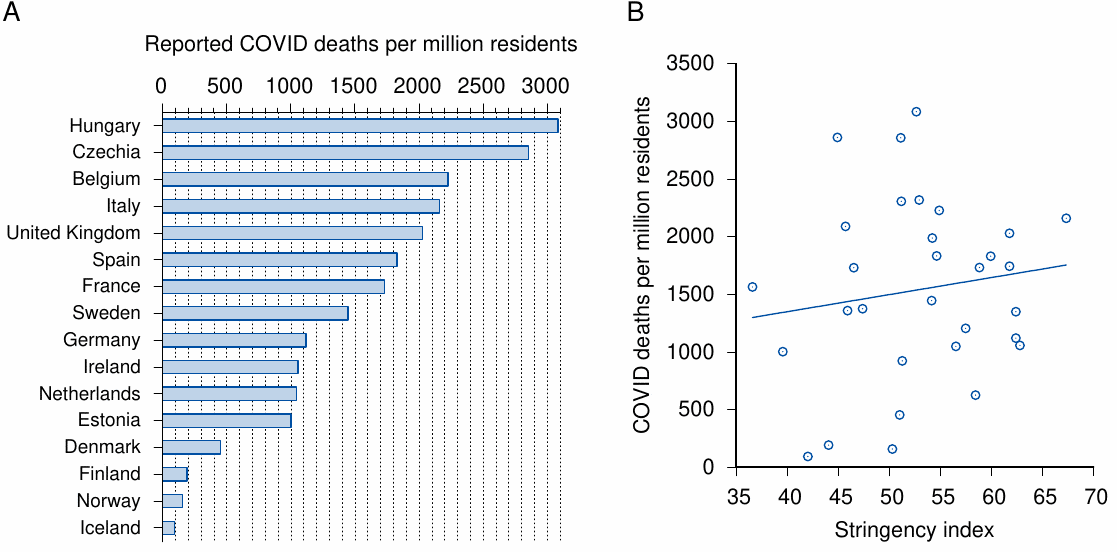
The lack of rigorous standards for determining the causes of death in diagnosed cases of the infection has produced a very large spread in the COVID mortality rates reported by different countries (Figure 3A). While some variation between countries must be expected, it surely is difficult to believe that the mortality in France, whose healthcare system is considered of very high quality, should be twenty times higher than in Iceland, or that Belgium should have five times more deaths per capita than Denmark.
The distortion apparent in these numbers makes it impossible to place any trust into those in panel B of the same figure. This graph shows the correlation—or rather, the lack thereof—between a “stringency index,” which summarizes the rigour of the lock-down and other measures imposed by national governments, and the reported COVID deaths. In this sample of 31 European countries (which includes the 16 countries represented in panel A), the correlation is very low, with an R2 value of only 0.02 (and a positive slope of the linear regression line). In other words, the quality of the mortality data is so low as to render the task of discerning any correlation between the stringency of lock-down measures and COVID mortality hopeless. In view of this deplorable quality of the raw data, it is unsurprising that proper epidemiological studies, too, fail to detect any benefits of more restrictive interventions [19,20].
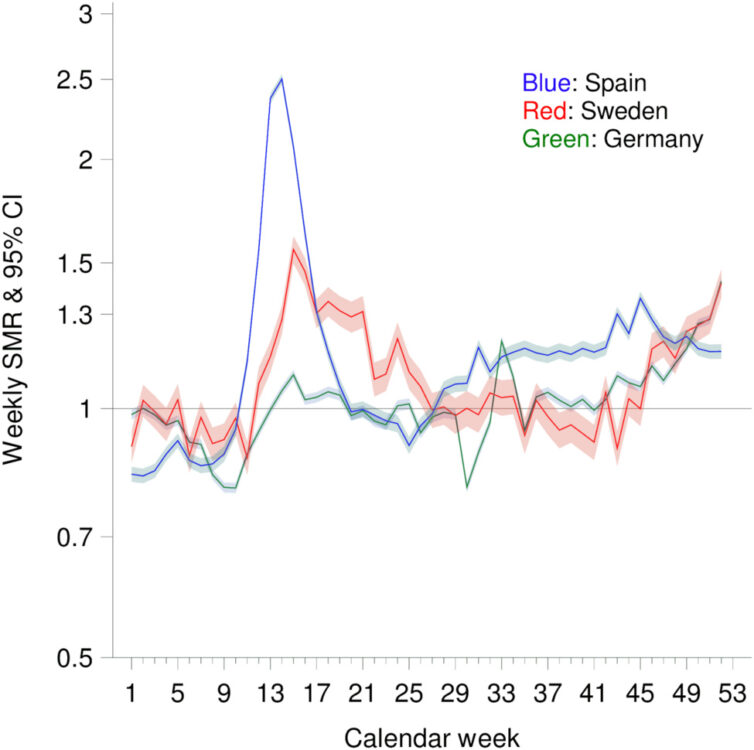
2.2. Lock-downs and overall mortality
We just saw that it is impossible to statistically detect any benefit of lock-downs and other mandates and restrictions imposed on the populace. The only recourse is to look at excess overall mortality during the “pandemic.” An instructive example is the comparison of three European countries provided by Kowall et al. [23]. In contrast to both Spain and Germany, Sweden never imposed any school closures or other hard “lock-down” measures, yet its standard mortality rate is unremarkable in comparison with these two other countries (see Figure 4). Kowall et al. also review possible causes for the observed excess mortalities in Spain and in Sweden, without however offering a definite conclusion regarding role of the lock-down measures. Obviously, no certain conclusions are possible in this regard based on the limited information available.
2.3. Do masks work?
A meta-analysis of 15 clinical studies by an international consortium of epidemiologists and infectious disease specialists offers the following conclusions [24]:
Compared to no masks there was no reduction of influenza-like illness (ILI) cases … or influenza … for masks in the general population, nor in healthcare workers … There was no difference between surgical masks and N95 respirators … Harms were poorly reported and limited to discomfort with lower compliance.
If no effect on disease transmission can be demonstrated even with the use of proper surgical or N95 masks, then surely the notion that those fashionable cloth masks will provide any benefit is fanciful. In conclusion, the evidence shows that masks don’t work.
We should note that influenza viruses and coronaviruses differ in some aspects of their biology from each other and from other “influenza-like” viral pathogens. However, all of these viruses are equivalent when it comes to airborne transmission—the viruses are exhaled with micro-droplets, which may or may not be inhaled by another person. The question as to whether a mask reduces transmission comes down simply to its ability to stop these micro-droplets, regardless of the identity of their viral cargo. Thus, the findings reported by Jefferson et al. are valid for COVID-19 as well.
A recent “cluster-randomized trial” conducted in Bangladesh claims to finally have unearthed the missing evidence to support the effectiveness of masks. The study was predictably covered with great fanfare in the mainstream press; it does, however, not stand up to scrutiny. The diagnostic method used in this study was an IgG antibody test, which is not suitable for diagnosing current or recent infections. Moreover, the study reports that the proportion of those with symptoms and a positive antibody test among the masked group was 0.76%, whereas in the unmasked group it was 0.68%. Passing off a reduction of 0.08% in an irrelevant diagnostic parameter as proof that masks reduce acute COVID infections is evidence not of mask effectiveness but of scientific incompetence, or worse. Rancourt [25] further dissects the many flaws of the study by Abaluck et al.
2.4. Is COVID likely to be transmitted outdoors?
It is well accepted that the risk of airborne transmission of infections is highest in indoor spaces that have limited ventilation with outdoor air [26–28]. Unlike the air in enclosed spaces, outdoor air will not stagnate or be recirculated, and it generally has a lower relative humidity, which will cause more rapid evaporation of exhaled micro-droplets. In addition, outdoors there is a higher level of ultraviolet radiation, which inactivates airborne microbes. Single-stranded RNA viruses such as SARS-CoV-2 are particularly sensitive to UV irradiation. Therefore, while to my knowledge no hard evidence exists to completely rule out outdoors transmission of COVID, the likelihood is certainly far lower than indoors. Thus, confining healthy people to their homes in order to ‘flatten the curve’ or ‘stop the spread of COVID’ is disproportionate and unreasonable.
2.5. Can clinically healthy people transmit COVID?
A subtext of the imposition of sweeping masking, distancing, or lock-down mandates on clinically healthy people is the idea of “asymptomatic spread”—persons who have been infected, but who show no signs of it other than a positive PCR test, are assumed to transmit this infection to other susceptible individuals. If we accept the idea of such asymptomatic spread, then the above drastic measures might indeed appear reasonable means for protecting those at risk.
It has, however, been unambiguously determined that such asymptomatic transmission is not relevant in practice. In a large-scale study, which involved almost 10 million Chinese residents, no new infections could be traced to persons that had tested positive for SARS-CoV-2 by PCR, but who did not exhibit any other signs of infection [29]. This agrees with several studies which compared PCR to virus isolation in cell culture among patients with acute COVID-19 disease. In all cases, growth of the virus in cell culture ceased as symptoms subsided, whereas PCR remained positive for weeks or months afterwards [30,31]. It was accordingly proposed to use cell culture rather than PCR to assess infectiousness and to determine the duration of isolation [31].
These findings indicate that restricting contact of persons at risk with those who show, or very recently showed, symptoms of acute respiratory disease would be effective and sufficient as a protective measure. Indiscriminately restricting the movements of persons who are not themselves at risk of severe disease, or of those who are currently asymptomatic is not required to achieve such protection.
2.6. COVID-19 can be treated effectively
A convergence of evidence indicates that early treatment of COVID-19 with existing drugs reduces hospitalisation and mortality by ~85% and 75%, respectively [32–36]. These treatment protocols include many tried and true antiviral, antiinflammatory, and anticoagulant medications, as well as monoclonal antibodies, zinc, and vitamins C and D. Two of the safest and most effective drugs for early treatment are ivermectin and hydroxychloroquine. Ivermectin, in particular, is generally considered so safe that it is often prescribed even in scabies, an unpleasant but harmless parasite disease of the skin that can be cured with topical treatment. It’s very strong inhibition of SARS-CoV-2 in vitro [37] can account for its observed clinical effectiveness.
The current restrictions and obstacles imposed by the WHO [38] and other authorities worldwide regarding the availability and distribution of these proven and safe drugs are scientifically and medically unjustifiable; they are simply more evidence of deliberate government malfeasance.
3. Lock-downs and children’s mental health
Kowalyshyn et al. have reviewed the literature on the effects of school closures, social distancing etc. on child mental health [39]. The authors note a very substantial increase of child suicides and suicide attempts in the year 2020. Here is the evidence. The Children’s Hospital of McMaster University in Hamilton, Ontario, reported an almost 300% increase in youth suicide attempts between October 2020 and January 2021, compared to the same time period one year before. The city of Pima, Arizona reported a 67% increase in child suicides during the 2020 lock-down, and Boston Children’s Hospital reported a 47% increase in children hospitalized for suicide attempts and suicide ideation between July and October 2020 compared to the same period in 2019.
These harrowing findings make it clear that the supposed pandemic control measures are not only unfit for their declared purpose, but that they are doing real harm to the health and sometimes even the lives of our children. Any such measures must be stopped immediately.
References
- Cucinotta, D. and Vanelli, M. (2020) WHO Declares COVID-19 a Pandemic. Acta biomed 91:157-160
- Doshi, P. (2011) The elusive definition of pandemic influenza. Bull. World Health Organ. 89:532-8
- Anonymous, (2009) Pandemic Influenza Preparedness and Response: A WHO Guidance Document.
- Rancourt, D. (2020) All-cause mortality during COVID-19: No plague and a likely signature of mass homicide by government response. (Unknown journal) (preprint)
- Ioannidis, J.P.A. (2020) Global perspective of COVID‐19 epidemiology for a full‐cycle pandemic. Eur. J. Clin. Invest. 50 (preprint)
- Ioannidis, J.P.A. (2021) Reconciling estimates of global spread and infection fatality rates of COVID‐19: An overview of systematic evaluations. Eur. J. Clin. Invest. 5:e133554
- Ioannidis, J.P.A. (2020) Infection fatality rate of COVID-19 inferred from seroprevalence data. Bull. World Health Organ. p. BLT.20.265892
- Anonymous, (2020) Report sulle caratteristiche dei pazienti deceduti positivi a COVID-19 in Italia. Il presente report è basato sui dati aggiornati al 17 Marzo 2020.
- Pueschel, K. (2020) Forensic Pathologist: No One in Hamburg Has Died of COVID-19 Alone.
- Anonymous, (2020) Bevölkerung nach Altersgruppen und Geschlecht.
- Axfors, C. and Ioannidis, J.P. (2021) Infection fatality rate of COVID-19 in community-dwelling populations with emphasis on the elderly: An overview. medRxiv (preprint)
- Bexte, K. (2020) CBC says this Manitoba hospital is OVERWHELMED by COVID—is it really? Keean Bexte investigates.
- Hartnett, K.P. et al. (2020) Impact of the COVID-19 Pandemic on Emergency Department Visits — United States, January 1, 2019-May 30, 2020. MMWR. Morbidity and mortality weekly report 69:699-704
- Kruizinga, M.D. et al. (2021) The impact of lockdown on pediatric ED visits and hospital admissions during the COVID19 pandemic: a multicenter analysis and review of the literature. Eur. J. Pediatr. 180:2271-2279
- Kuitunen, I. et al. (2020) The effect of national lockdown due to COVID-19 on emergency department visits. Scand. J. Trauma Resusc. Emerg. Med. 28:114
- Ojetti, V. et al. (2020) Non-COVID Diseases during the Pandemic: Where Have All Other Emergencies Gone?. Medicina 56 (preprint)
- Rennert-May, E. et al. (2021) The impact of COVID-19 on hospital admissions and emergency department visits: A population-based study. PLoS One 16:e0252441
- Salerno, M. et al. (2020) No Autopsies on COVID-19 Deaths: A Missed Opportunity and the Lockdown of Science. J. Clin. Med. 9 (preprint)
- Bendavid, E. et al. (2021) Assessing mandatory stay‐at‐home and business closure effects on the spread of COVID‐19. Eur. J. Clin. Invest. 51 (preprint)
- De Larochelambert, Q. et al. (2020) Covid-19 Mortality: A Matter of Vulnerability Among Nations Facing Limited Margins of Adaptation. Frontiers in public health 8 (preprint)
- Anonymous, (2021) Incidence of coronavirus (COVID-19) deaths in the European Economic Area and the United Kingdom as of September 19, 2021, by country.
- Anonymous, (0) COVID-19 Government Response Tracker.
- Kowall, B. et al. (2021) Excess mortality due to Covid-19? A comparison of total mortality in 2020 with total mortality in 2016 to 2019 in Germany, Sweden and Spain. PLoS One 16:e0255540
- Jefferson, T. et al. (2020) Physical interventions to interrupt or reduce the spread of respiratory viruses. Part 1—Face masks, eye protection and person distancing: systematic review and meta-analysis. medRxiv (preprint)
- Rancourt, D. (2021) Do Face Masks Reduce COVID-19 Spread in Bangladesh? Are the Abaluck et al. Results Reliable?.
- Knibbs, L.D. et al. (2011) Room ventilation and the risk of airborne infection transmission in 3 health care settings within a large teaching hospital. American journal of infection control 39:866-72
- Morawska, L. and Milton, D.K. (2020) It Is Time to Address Airborne Transmission of Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 71:2311-2313
- de Man, P. et al. (2021) Outbreak of Coronavirus Disease 2019 (COVID-19) in a Nursing Home Associated With Aerosol Transmission as a Result of Inadequate Ventilation. Clin. Infect. Dis. 73:170-171
- Cao, S. et al. (2020) Post-lockdown SARS-CoV-2 nucleic acid screening in nearly ten million residents of Wuhan, China. Nat. Commun. 11:5917
- Wölfel, R. et al. (2020) Virological assessment of hospitalized patients with COVID-2019. Nature 581:465-469
- Basile, K. et al. (2020) Cell-based culture of SARS-CoV-2 informs infectivity and safe de-isolation assessments during COVID-19. Clin. Infect. Dis. (preprint)
- Orient, J. et al. (2020) A Guide to Home-Based COVID Treatment.
- McCullough, P.A. et al. (2020) Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19). Reviews in cardiovascular medicine 21:517-530
- Procter, B.C. et al. (2021) Early Ambulatory Multidrug Therapy Reduces Hospitalization and Death in High-Risk Patients with SARS-CoV-2 (COVID-19). International journal of innovative research in medical science 6:219-221
- McCullough, P.A. et al. (2021) Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection. Am. J. Med. 134:16-22
- Anonymous, (2020) Real-time database and meta analysis of 588 COVID-19 studies.
- Caly, L. et al. (2020) The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 178:104787
- Anonymous, (2021) WHO advises that ivermectin only be used to treat COVID-19 within clinical trials.
- Kowalyshyn, J. and Alexander, P.E. (2021) Deaths of Despair: Child suicde evidence package.
