Daily Wins
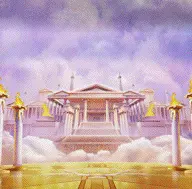
Olympus x1000

Starlight Princess

Sweet Bonanza

Supper Scatter

MJ 3

Mahjong Ways
Popular Games

Mafia Mayhem

Wild Bandito

Treasures Aztec

Chronicles

Silverback

Elven Gold
Hot Games

Big Pot

Pragmatic Play

Play n Go

Reel Kingdom

Spinix

Yggdrasil

